"Shin splints" is considered to be a catch-all term that encompasses injuries such as muscle tears and stress fractures. However, in my practice, I stick to calling those things "muscle tears and stress fractures". As far as I'm concerned, shin splints (or medial tibial stress syndrome) involves tightness and restriction of the calf muscles muscles to the point that they pull strongly enough on the tibia (shin bone) to cause inflammation. This effect occurs when the outermost layer that covers the bone - the periosteum - is lifted up due to this tension, allowing the inflammation to develop underneath. Oftentimes, there are microtears throughout the calf muscles involves as well as pain referred through the entire medial calf. Sounds awful, huh?
Here's where I start to get more general and provide a list of the go-to-reasons why you may have MTSS and what you can do about it. Keep in mind, this training advice, not medical. If you have a real problem, seek help from a medical professional in person.
1) You're a Heel Runner
If, when you run, you strike the ground heavily with your heel, the hard impact could be a likely trigger for the inflammation beneath your periosteum if you've already been prone to it. The strike of the heel allows all the force to travel directly up your leg, causing impact-related problems all the way up to the back. Retraining of your running gait, switching to a softer running surface, or wearing a flatter running shoe that promotes more midfoot running are excellent places to start for your recovery.
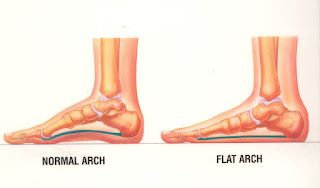
2) You're a Pronator and/or Flat-Footed
If your feet have very little natural arch of if you have an exaggerated inward-roll of your feet while walking and running, this could be putting excessive strain through the medial calf muscle. Often, improper shoe support is the cause, and you may need more added to support the arch and stop the pronation. You may also need less as well. I, myself, self-corrected once I switched to minimalist shoes and no longer had an artificial arch causing my foot to roll in. Foot exercises can also help to lift the arch in your foot naturally as well, to an extent.3) Your Butt is Asleep
If your glutes are inactive during gait (they should be the primary muscle moving you along), then the hamstrings and calves tend to take over. If you're getting your calves to take on the workload that your much stronger gluteal muscles should normally be handling, then you'll definitely see tightness and restriction through the muscles occur as a result.4) You're Doing Calf Raises
Firstly, I hope that no one save for bodybuilding and fitness competitors are doing calf raises. Your calves were designed to run for hours, not lifting a heavy weight ten times. So that's your first problemSecondly, most-often when someone does a calf raises, they are pronating and favouring the medial calf overall, causing it to become more stronger - and tighter - than the outer as a result. If you really have to do calf raises, try squeezing a tennis ball between your heels to help distribute the load.
5) You're Stretching Improperly
If you're stretching your calves to try to relieve your pain but are getting no results, recheck your technique. If you're doing the traditional runners stretch by lunging against a wall, pushing your toes up against the wall, or dropping your heel off a step, you may very well be moving into pronation again. Try doing the runner's lunger, but with the foot flat on an incline to keep the leg and foot properly aligned.Furthermore, are you stretching your entire calf? When stretching, you need to do both a straight-legged stretch for the more superficial gastrocnemius muscle (which crosses the knee) and one with a slightly bent knee to get the deeper soleus which crosses the ankle only.
6) You're Not "Born to Run"
Finally, maybe you just have anatomy against you. I don't care what some people say; we're not all naturally built to run long distances. Yes, we all did it when we were cavemen, but do you really think that our anatomy hasn't at all changed since cro magnons walked the earth? If you're naturally (or unnaturally) heavy-set and have short legs relative to your weight and height, it may just be too much for your legs to handle running a marathon without extensive and specific training. I'll never say that there's a physical feat that anyone can't accomplish, but without a doubt, it's going to be a much harder time for some than others.Take from this what you will. Everyone's body is different though, so the reason for your pain may very well not have been mentioned. Use it as a starting point. It may take trial and error, but no one is meant to suffer without a solution.